- 2023.11.08.
- By: hkwebdesign
- No Comments
What is the HPV virus?
HPV is the most common sexually transmitted pathogen that affects both sexes. 80% of sexually active adults will experience the infection during their lifetime.
The most serious consequence of HPV infection is the development of various cancerous changes caused by the virus – cervical cancer, vaginal, oral cavity, throat, penile and rectal cancer. These diseases typically develop over many years.
Why is HPV screening important?
With regular HPV screening tests, HPV type infection with a high cancer risk can be detected in time, so it is possible to prevent the development of cancerous lesions.
When is the examination necessary?
Over the age of thirty, HPV screening is nowadays recommended as a cervical screening, while at younger ages a traditional cytological examination is preferred. The reason for this is that chances for HPV infection is very high under the age of 30 (surveys showed 20-25 percent HPV infection in case of sexually active girls aged 20-25), so there would be many positive results that show the virus DNA, however these results does not represent an increased risk. This is based on the fact that HPV infection is typically only temporary at this age, while the risk of cancer increases only by the persistent HPV condition.
The infection is more likely to be permanent after the age of 30-35, thus increasing the risk of cancer – this is the reason why the HPV screening makes sense at this age.
Who do we recommend taking the test?
HPV infection can affect any sexually active person. Frequent changes of partners increases the risk, if protection against possible infection was not satisfactory during cohabitation or if a person maintains sexual relations with several partners at the same time.
Since the infection can exist without symptoms, it is recommended to take the test even in the absence of symptoms, in this way you can prevent your current or new partner from passing the infection unnoticed.
Do not perform the test during pregnancy and 3 months after birth, during menstruation, or while using a vaginal product.
When should you take the test?
If you associate the possibility of infection with a specific event, take the test after the end of the window period. The reason for this is that during the window period the presence of the given pathogen cannot be confirmed by diagnostic methods, so the laboratory test carried out during this period may give false negative results.
Testing during the window period is not reliable, so in this case, repeated sampling after the end of the window period can be recommended.
The window period for human papillomavirus infection is 2-3 months. In most cases, HPV infection goes unnoticed and asymptomatic in both sexes, and then goes away on its own. But since you can catch the infection again and again, we recommend that you get tested regularly to prevent complications from HPV.
What does the HPV test look for?
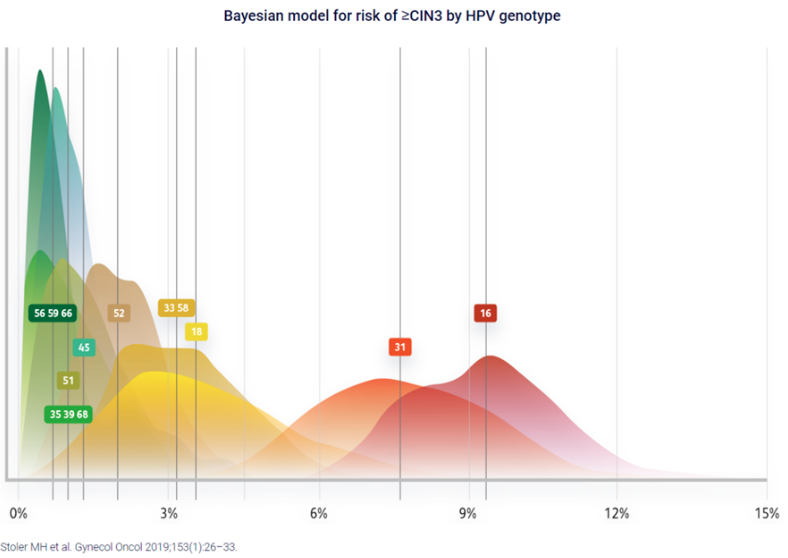
Figure 1. Stratified risk of high-grade cervical disease using HPV extended genotyping in women, ≥25 years of age, with NILM cytology
The test examines the presence of high-risk types of HPV in the area of the vaginal mucosa.
In the laboratory of the Promedical Center clinic, we are able to perform world-class tests. We can detect and identify 19 high-risk HPV genotypes and 9 low-risk HPV genotypes using the real-time PCR method from cervical samples.
The analyses are carried out by our specialists in the central laboratory of Promedical group (the Pro-Vitam molecular biology laboratory in Sfantu Gheorghe).
HPV screening is a screening test that can be used to detect the presence of the human papilloma virus in the vagina and cervix. During the examination, we can also determine the type of the given virus strain, which reveals whether the particular strain means high risk and it can cause cervical cancer or cervical cancer in the long term.
HPV 16 and HPV 18 are the most common cause of cervical cancer, but HPV 26, 31, 33, 35, 39, 45, 51, 52, 53, 56, 58, 59, 66 are at high risk. , 68, 69, 73, 82 strains as well. Of course, we also test for low-risk strains, these are: 6, 11, 40, 42, 43, 44, 54, 61, 70.
Stratified risk of high-grade cervical disease using HPV extended genotyping in women, ≥25 years of age, with NILM cytology
How accurate are the HPV screening results?
A negative HPV test gives an almost 100 percent result, so HPV infection can practically be ruled out with screening. In such cases, a cancer-preventing condition will most certainly not develop in the next 3 years, but even within 5 years, the chance is only a few tenths of a percent.
Why HPV screening is needed, in addition to the traditional smear test?
If a traditional smear was taken and the HPV test yielded a negative result (i.e. the presence of high-risk HPV virus would not be revealed), the risk of developing a pre-cancerous condition within 3 years would still be almost 40 percent despite the negative finding. For this reason, the need for HPV screening over the age of 30 has come to the fore.
How is sampling carried out?
The examination can be performed by a gynecologist, but there are also self-sampling procedures that can be reliably used at home. In both cases, the sample is analysed in a laboratory. Before taking the sample, take into account that it should not take place during menstruation, and that no foreign substances or chemicals should be in the vagina. Douche should not be used before sampling, but general hygiene should be observed.
What to do after receiving the result?
If your result is positive – avoid further sexual contact and see your specialist as soon as possible. The results of the test must be evaluated together with the entire clinical picture, for which you can ask for the advice of a dermatologist and gynecologist or a urologist, depending on the area of sampling.
If the result of the test is negative, the test could not prove the presence of the tested pathogens in your case at the time of sampling in the given sampling region.
If the test result is negative, but you or your partner experience symptoms typical of an STI infection, also seek the help of a specialist.
Since the STI infections examined by the test do not develop lasting immunological protection in the body, you may be infected again with the given or other STI pathogen in the event of a previous positivity.
Who can’t be tested?
HPV screening is completely pointless in case children and under 30 years of age. In the case of the latter, it is unnecessary to carry out the examination because in their case the infection is very common, but not permanent, so it does not represent an actual risk in terms of tumour formation.
Source:
- Stoler MH et al. Am J Clin Pathol. 2019;151(4):433–42.
- Bonde JH et al. J Low Genit Tract Dis. 2020;24(1):1–13.
- Monsonego J et al. Gynecol Oncol. 2015;137(1):47-54.
- Perkins RB et al. J Low Genit Tract Dis. 2020;24:102–31.
- Bonde J et al. Int J Cancer. 2019;145:1033–41.
- Schiffman M et al. Gynecol Oncol. 2015;138(3):573–8.
- Schiffman M et al. Int J Cancer. 2016:139:2606–15.
- Schiffman M et al. J Clin Microbiol. 2015;53(1):52–9.
https://womens-health-solutions.bd.com/cervical-cancer/extended-genotyping/hpv-31-identification