- 2020.07.30.
- By: hkwebdesign
- No Comments
Breast Cancer
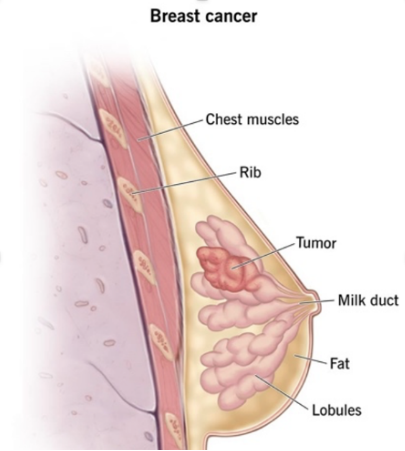
Breast cancer tumors develop when breast cells mutate and grow.
What is breast cancer?
Breast cancer originates in your breast tissue. It occurs when breast cells mutate (change) and grow out of control, creating a mass of tissue (tumor). Like other cancers, breast cancer can invade and grow into the tissue surrounding your breast. It can also travel to other parts of your body and form new tumors. When this happens, it’s called metastasis.
Who is mainly affected by breast cancer?
Although breast cancer is one of the most common cancers among women (second only to skin cancer), often diagnosed over the age of 50, this type of cancer is currently the most curable one too, especially if detected in time.
Although its rare among men, but breast cancer can affect them as well with a much rapid and worse disease course.
How common is breast cancer?
In the United States for example, breast cancer is the second-leading cause of cancer death in women, after lung cancer. It’s also the leading cause of cancer death among women ages 35 to 54. Breast cancer is one of the most common cancers in Hungary. Approximately 5,000 to 6,000 new breast cancer patients are registered each year and the disease causes the death of approximately 2,000 women. That is, almost every 10th woman develops this disease during her lifetime. These results definitely seem scary in the light of what we wrote earlier, according to which this is currently the most curable cancer, especially with the help of the mammogram early detection.
What are the early signs of breast cancer?
Breast cancer symptoms can vary for each person. Possible signs of breast cancer include:
- A change in the size, shape or contour of your breast.
- A mass or lump, which may feel as small as a pea.
- A lump or thickening in or near your breast or in your underarm that persists through your menstrual cycle.
- A change in the look or feel of your skin on your breast or nipple (dimpled, puckered, scaly or inflamed).
- Redness of your skin on your breast or nipple.
- An area that’s distinctly different from any other area on either breast.
- A marble-like hardened area under your skin.
- A blood-stained or clear fluid discharge from your nipple.
Some people don’t notice any signs of breast cancer at all. That’s why routine mammograms and are so important.
What causes breast cancer?
Experts don’t know exactly what causes this process to begin in the first place. However, research indicates that are several risk factors that may increase your chances of developing breast cancer. These include:
- Age. Being 55 or older increases your risk for breast cancer.
- Sex. Women are much more likely to develop breast cancer than men.
- Family history and genetics. If you have parents, siblings, children or other close relatives who’ve been diagnosed with breast cancer, you’re more likely to develop the disease at some point in your life. About 5% to 10% of breast cancers are due to single abnormal genes that are passed down from parents to children, and that can be discovered by genetic testing.
- Smoking. Tobacco use has been linked to many different types of cancer, including breast cancer.
- Alcohol use. Research indicates that drinking alcohol can increase your risk for certain types of breast cancer.
- Obesity. Having obesity can increase your risk of breast cancer and breast cancer recurrence.
- Radiation exposure. If you’ve had prior radiation therapy — especially to your head, neck or chest — you’re more likely to develop breast cancer.
- Hormone replacement therapy. People who use hormone replacement therapy (HRT) have a higher risk of being diagnosed with breast cancer.
There are many other factors that can increase your chances of developing breast cancer.
We propose to contact Pro Medical to find out if you’re at risk.
PREVENTION
How can I be sure that my cancer will be detected before it has spread?
While you can’t prevent breast cancer altogether, there are certain things you can do to reduce your risk of discovering it at an advanced stage. For example:
- Get routine mammograms Cancer Societies all over the world recommends having a baseline mammogram at age 35, and a screening mammogram every year after age 40.
- Examine your breasts every month after age 20. You’ll become familiar with the contours and feel of your breasts and will be more alert to changes.
- Have your breasts examined by a healthcare provider at least once every three years after age 20, and every year after age 40.
DIAGNOSIS AND TESTS
How is breast cancer diagnosed?
First of all its you, who can regurarily check your breast and find any abnormalities yourself.
So that you can easily recognize the symptoms, we list the most common ones below:
- Changes in the surface of the skin on or around the breast: Wrinkling. A lump in the breast can cause the connective tissue fibers to shorten and the skin to retract, resulting in a wrinkled or dented appearance.
- Changes in the surface of the skin on or around the breast: Cellulite. Small indentations on the skin of the breast may indicate blockage of the breast’s lymphatic vessels. This causes inflammation and swelling of the breast tissue, which results in the formation of small pits that look like the orange peels on a larger surface of the skin. In some cases, this change can be a symptom of a type of breast cancer, inflammatory breast tumor.
- Visible veins on the surface of the breast. It may indicate vascular occlusion, which may indicate a cancerous lump or the increased blood supply associated with the growth of the breast tumor.
- Eczema-like rash or redness on or around the nipple. This is a very rare symptom of breast cancer. In some cases, it is associated with a disease related to breast cancer, Paget’s disease.
- Inversion of the nipple or changes in its position and shape. Behind a permanently inverted nipple, there may be a cancerous lump pulling it in.
- Discharge of the nipple without pushing it or squeezing it. This may indicate that the tiny milk ducts behind the nipple are lined with cancer cells.
- Firmer-feeling breast tissue: This may indicate a lump in the milk-producing gland, but it may also be a sign of blocked lymphatic vessels.
- Swelling in the armpit. This may indicate a lump in the axillary lymph nodes. Sometimes an armpit lump can be more noticeable and easier to spot than a lump in the breast.
Pro Medical will perform a breast examination and ask about your family history, medical history and any existing symptoms. In Pro Medical you also have the possiblity to perform a Genetic Screening examination, that is to inverstigate your genetic determinations to eg. A breast cancer. It is also recommended to tests and check for breast abnormalities. These tests may include:
- Mammogram. These special X-ray images can detect changes or abnormal growths in your breast. A mammogram is commonly used in breast cancer prevention.
- Ultrasonography. This test uses sound waves to take pictures of the tissues inside of your breast. It’s used to help diagnose breast lumps or abnormalities.
- Positron emission tomography (PET) scanning: A PET scan uses special dyes to highlight suspicious areas. During this test, your healthcare provider injects a special dye into your veins and takes images with the scanner.
- Magnetic resonance imaging (MRI): This test uses magnets and radio waves to produce clear, detailed images of the structures inside of your breast.
If we are trying to decide whether a breast ultrasound or a mammogram is the right choice for you, we will consider your health and family history, the reason for the study, and how the strengths and weakness of each option may affect the result in your case.
Mammogram
- Uses a small amount of radiation
- Can’t distinguish between a cyst and a solid mass
- Not as good at spotting abnormalities in people with dense breast tissue
- Good at spotting calcifications
- Different views can give the radiologist a look at the entire breast
- Can be used to find suspicious areas deeper inside the breast
- Can view the axillary lymph nodes
- Typically used for breast cancer screening
Ultrasound
- Does not use radiation
- Better availability compared to mammography
- Can help distinguish between solid masses and cysts
- Better at spotting abnormalities in people with dense breast tissue
- Much less effective at finding calcifications
- Cannot view the entire breast
- Cannot view deep breast tissue
- Cannot view the axillary lymph nodes
- Typically used for diagnosing abnormalities found during screening
Breast Density
Having dense breasts makes finding breast cancer more difficult and increases the risk of developing breast cancer.
Having a mammogram, ultrasound, and possibly an MRI can improve the accuracy of breast cancer screening for people with dense breasts.
If we see anything suspicious on the imaging tests, we may take a biopsy of your breast tissue. We’ll send the sample to a pathology lab for analysis.
OUTLOOK / PROGNOSIS
What can I expect if I have breast cancer?
If you’ve been diagnosed with breast cancer, your healthcare provider will talk with you in detail about your treatment options. Treatment and recovery will be different for everyone, so they can tell you what to expect in your situation.
Is breast cancer fatal?
People with early-stage breast cancer often manage their condition successfully with treatment. In fact, many people who’ve received a breast cancer diagnosis go on to live long, fulfilling lives. Late-stage breast cancer is more difficult to treat, however, and can be fatal.
What is the survival rate for breast cancer?
The overall five-year survival rate for breast cancer is 90%. This means that 90% of people diagnosed with the disease are still alive five years later. The five-year survival rate for breast cancer that has spread to nearby areas is 86%, while the five-year survival rate for metastatic breast cancer is 28%. Fortunately, the survival rates for breast cancer are improving as we learn more about the disease and develop new and better approaches to management.
Keep in mind that survival rates are only estimates. They can’t predict the success of treatment or tell you how long you’ll live. If you have specific questions about breast cancer survival rates, talk to your healthcare provider.
When should I see my healthcare provider?
In addition to having routine checkups and mammograms, you should call your healthcare provider if you notice any changes in your breasts.
What questions should I ask my healthcare provider?
Learning everything you can about your diagnosis can help you make informed decisions about your health. Here are some questions you may want to ask your healthcare provider:
- Where is the tumor located?
- Has the tumor spread?
- What stage breast cancer do I have?
- What do the estrogen receptor (ER), progesterone receptor (PR) and HER2 tests show and what do the results mean for me?
- What are my treatment options?
- Is breast cancer surgery an option for me?
- Will I be able to work while I undergo treatment?
- How long will my treatment last?
- What other resources are available to me?
What are the breast cancer stages?
Staging helps describe how much cancer is in your body. It’s determined by several factors, including the size and location of the tumor and whether the cancer has spread to other areas of your body. The basic breast cancer stages are:
- Stage 0. The disease is non-invasive. This means it hasn’t broken out of your breast ducts.
- Stage I. The cancer cells have spread to the nearby breast tissue.
- Stage II. The tumor is either smaller than 2 centimeters across and has spread to underarm lymph nodes or larger than 5 centimeters across but hasn’t spread to underarm lymph nodes. Tumors at this stage can measure anywhere between 2 to 5 centimeters across, and may or may not affect the nearby lymph nodes.
- Stage III. At this stage, the cancer has spread beyond the point of origin. It may have invaded nearby tissue and lymph nodes, but it hasn’t spread to distant organs. Stage III is usually referred to as locally advanced breast cancer.
- Stage IV. The cancer has spread to areas away from your breast, such as your bones, liver, lungs or brain. Stage IV breast cancer is also called metastatic breast cancer.
MANAGEMENT AND TREATMENT
How is breast cancer treated?
There are several breast cancer treatment options, including surgery, chemotherapy, radiation therapy, hormone therapy, immunotherapy and targeted drug therapy. What’s right for you depends on many factors, including the location and size of the tumour, the results of your lab tests and whether the cancer has spread to other parts of your body. Your healthcare provider will tailor your treatment plan according to your unique needs. It’s not uncommon to receive a combination of different treatments, too.
Breast cancer surgery
Breast cancer surgery involves removing the cancerous portion of your breast and an area of normal tissue surrounding the tumour. There are different types of surgery depending on your situation
Chemotherapy for breast cancer
We may recommend chemotherapy for breast cancer before a lumpectomy in an effort to shrink the tumour. Sometimes, it’s given after surgery to kill any remaining cancer cells and reduce the risk of recurrence (coming back). If the cancer has spread beyond your breast to other parts of your body, then we may recommend chemotherapy as a primary treatment.
Radiation therapy for breast cancer
Radiation therapy for breast cancer is typically given after a lumpectomy or mastectomy to kill remaining cancer cells. It can also be used to treat individual metastatic tumours that are causing pain or other problems.
Hormone therapy for breast cancer
Some types of breast cancer use hormones — such as estrogen and progesterone — to grow. In these cases, hormone therapy can either lower estrogen levels or stop estrogen from attaching to breast cancer cells. Most often, healthcare providers use hormone therapy after surgery to reduce the risk of breast cancer recurrence. However, they may also use it before surgery to shrink the tumour or to treat cancer that has spread to other parts of your body.
Immunotherapy for breast cancer
Immunotherapy uses the power of your own immune system to target and attack breast cancer cells. Treatment is given intravenously (through a vein in your arm or hand). We might use immunotherapy for breast cancer in combination with chemotherapy.
Targeted drug therapy for breast cancer
Some drugs can target specific cell characteristics that cause cancer. We might recommend targeted drug therapy in cases where breast cancer has spread to other areas of your body. Some of the most common drugs used in breast cancer treatment include monoclonal antibodies, antibody-drug conjugates and kinase inhibitors.
Our note:
Being diagnosed with breast cancer can feel scary, frustrating and even hopeless. If you or a loved one is facing this disease, it’s important to take advantage of the many resources available to you. Talk to your healthcare provider about your treatment options. You may even want to get a second opinion before making a decision. You should feel satisfied and optimistic about your treatment plan. Finally, joining a local support group can help with feelings of isolation and allow you to talk with other people who are going through the same thing.
Sources:
- Verywellhealth, Serenity Mirabito RN, OCN Breast Ultrasound vs. Mammography: Which Is Best?
- Cleveland Clinic
- Házipatika